Dysplasia is a term that refers to abnormal growth or development of an organ or tissue. When we talk about hip dysplasia, we are referring to the abnormal development of the “ball” of the thighbone (femoral head) and the hip “socket” (acetabulum) relative to one another. This is also known as Developmental Dysplasia of the Hip (DDH).
Normally, the hip joint is quite stable, with the head of the femur firmly positioned inside the acetabulum. Hip dysplasia occurs when the acetabulum is shallow and doesn’t provide sufficient coverage of the femoral head, causing instability of the hip joint. Hip dysplasia is thought to be due to a predisposition of soft tissue laxity (looseness) which causes the femoral head to move away from the hip socket during childhood. If this malalignment is not addressed successfully in early childhood with casts or bracing, the acetabulum can develop an irregular, shallow and upsloping shape in response to the abnormal position of the femoral head. This in turn leads to a deformity of the acetabulum that persists into adolescence and adulthood. Without a normal “socket” to sufficiently cover and stabilize the “ball”, the femoral head can partially or even completely dislocate from the hip socket over time.
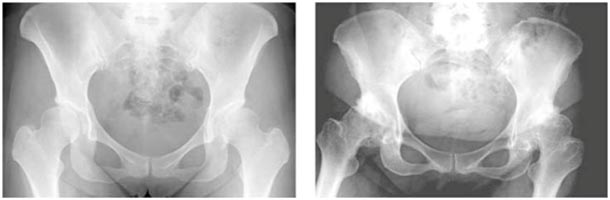
Hip dysplasia that is untreated can cause significant disability for patients including hip pain, labral tears, and progression to hip arthritis at a young age. The following image shows a 30-year-old female with hip pain and early hip dysplasia (left) and a 49-year-old female with underlying hip dysplasia (right) with progression to full-blown advanced hip osteoarthritis. The woman on the right has since undergone total hip replacement on both sides.
Treatment
Here at the Joint Preservation Institute, we strive to intervene long before hip replacement becomes necessary. It is our philosophy that your native joint is far superior to any mechanical joint that may replace it. Dr. Jamali has extensive experience with surgeries that can correct the dysplastic anatomy, treat your hip pain, and prevent progression to secondary hip osteoarthritis.
Periacetabular Osteotomy
The Bernese Periacetabular Osteotomy (PAO) has proven to be a safe and effective joint-preserving treatment for young adults with symptomatic hip dysplasia and no osteoarthritis. This procedure was first developed by Dr. Reinhold Ganz in 1983, an orthopedic surgeon with whom Dr. Jamali trained during his Hip Preservation Surgery Fellowship in 2002. The procedure involves making a series of angular cuts on the pelvis, separating the hip socket from the pelvis and allowing free rotation of the socket in three dimensions. It has proven to be one of the most effective surgical procedures in the treatment of hip dysplasia in adults. The major advantage of the procedure is the flexibility of placement of the hip socket in essentially any position and the preservation of the stability of the pelvic ring. The ability to freely position the hip socket gives your surgeon the ability to customize the correction of the anatomy to the specific deficiencies of that pelvis.
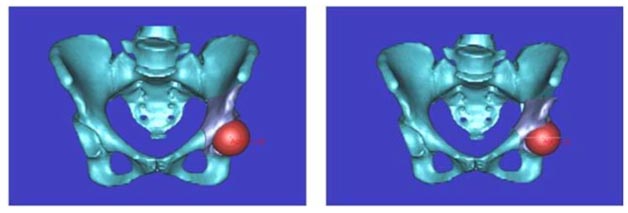
At the Joint Preservation Institute, we have been using three dimensional reconstructions to make a very precise computer model of the pelvis. With this information and a large database of normal pelvis models, we are able to plan the reorientation of the hip socket to as close a normal position as possible even before the operation. The preoperative computer plan is correlated with intraoperative x-rays which allow for a very precise correction. The other benefit of the PAO is the innate stability of the hip socket at the end of the procedure. Overall, if the hip has little to no arthritis, the success rate for avoiding a hip replacement is greater than 90% for at least ten years if not longer.
Hip Arthroscopy
As the practice of hip arthroscopy has expanded, there has been increasing interest in the role of arthroscopic treatment as a less invasive surgical technique and in patients with less severe forms of hip dysplasia. Hip arthroscopy is a minimally invasive surgery during which a small camera is inserted into the hip joint through tiny incisions. The camera projects an image of the inside of the joint onto a large screen monitor allowing Dr. Jamali to look for any damage, assess the type of injury, and repair the problem.

A common problem associated with hip dysplasia is a labral tear. The hip labrum is a cartilaginous ring that surrounds the outside rim of your hip joint socket. In a patient with joint instability due to hip dysplasia, there is increased stress placed on the acetabular rim where the labrum resides. In one systematic review, labral tears were seen in 56% of patients who underwent a PAO for hip dysplasia. Interestingly, this study also found that arthroscopy was better at identifying labral tears and chondral injury when compared to open arthrotomy1.
It is therefore natural to wonder if a hip arthroscopy might be a better surgical option than a PAO for hip dysplasia. Unfortunately, studies have not been so promising. While arthroscopy is a fantastic option for treating isolated labral tears and bony impingement deformities, it does not address the underlying structural abnormality of hip dysplasia. In fact, isolated hip arthroscopy has been associated with high rates of treatment failure, post-operative subluxations/dislocations, and rapidly progressive hip arthritis in some cases2,3,4,5.
Nevertheless, a newer arthroscopic procedure for hip dysplasia—capsular plication—has shown some promise6. During this surgery, an arthroscopic a labral debridement, repair, or reconstruction is performed as necessary. At the end of the procedure, the hip capsule (a strong, dense sheet of fibrous tissue that surrounds the hip joint) is sown up tightly, to provide additional stability. This may be a good option for young patients with so-called “borderline” hip dysplasia, who have evidence of labral damage in the setting of only mild acetabular under-coverage.
Finally, hip arthroscopy may be combined with a PAO surgery at the same time. Theoretically, this would combine the excellent labrum-repairing-potential of a hip arthroscopy with the structural-correction-capabilities of a PAO. Although early studies have shown outcomes worthy of optimism, high-level evidence for the efficacy of combined procedures is currently lacking7,8,9,10.
Femoral Osteotomy
In addition to early arthritis and labral tears, hip dysplasia may also be associated with a rotational condition of the thighbone (femur) known as femoral anteversion. Femoral neck anteversion is a measurement of the angle between the longitudinal axis of the femoral neck and the axis passing horizontally through the femoral condyles at the knee. When this angle is too large (greater than about 20 degrees), there is a compensatory internal rotation of that femur. This rotational variation typically results in a “pigeon-toed” gait, in which the toes of the affected side point inward.
To treat this rotational malalignment, a surgery known as a femoral osteotomy may be performed along with the PAO. In a femoral osteotomy, a transverse bone cut (osteotomy) is made just below the lesser trochanter of the femur. The distal portion of the thighbone is then precisely de-rotated externally by a specific degree, as predetermined in pre-operative planning, and the bone is fixed in that position. While the PAO addresses the stability and congruency of the hip joint, the femoral osteotomy restores the natural alignment of the limb as a whole.
References
1. Redmond JM, Gupta A, Stake CE, Domb BG. The prevalence of hip labral and chondral lesions identified by method of detection during periacetabular osteotomy: arthroscopy versus arthrotomy. Arthroscopy. 2014;30(3):382–8.
2. Benali Y, Katthagen BD. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy. 2009;25(4):405–7.
3. Matsuda DK, Khatod M. Rapidly progressive osteoarthritis after arthroscopic labral repair in patients with hip dysplasia. Arthroscopy. 2012;28(11):1738–43.
4. Mei-Dan O, McConkey MO, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28(3):440–5.
5. Duplantier NL, McCulloch PC, Nho SJ, Mather RC, Lewis BD, Harris JD. Hip dislocation or subluxation after hip arthroscopy: a systematic review. Arthroscopy. 2016;32(7):1428–34.
6. Domb BG, Chaharbakhshi EO, Perets I, Yuen LC, Walsh JP, Ashberg L. Hip arthroscopic surgery with labral preservation and capsular plication in patients with borderline hip dysplasia: minimum 5-year patient-reported outcomes. Am J Sports Med. 2018;46(2):305–13.
7. Domb BG, Domb B, LaReau J, Redmond JM. Combined hip arthroscopy and periacetabular osteotomy: indications, advantages, technique, and complications. Arthrosc Tech. 2014;3(1):e95–e100.
8. Nakayama H, Fukunishi S, Fukui T, Yoshiya S. Arthroscopic labral repair concomitantly performed with curved periacetabular osteotomy. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):938–41.
9. Sabbag CM, Nepple JJ, Pascual-Garrido C, Lalchandani GR, Clohisy JC, Sierra RJ. The addition of hip arthroscopy to periacetabular osteotomy does not increase complication rates: a prospective case series. Am J Sports Med. 2019;47(3):543–51.
10. Ricciardi BF, Fields KG, Wentzel C, Kelly BT, Sink EL. Early functional outcomes of periacetabular osteotomy after failed hip arthroscopic surgery for symptomatic acetabular dysplasia. Am J Sports Med. 2017;45(11):2460–7.
