Dr Jamali’s PAO Journey
Periacetabular osteotomy (PAO) is a remarkable surgical procedure developed for the treatment of a variety of hip abnormalities requiring repositioning of the hip socket or acetabulum. It has gained widespread use but there are still many myths and misunderstandings about the procedure. In the following pages, I hope to take you through the history of the periacetabular osteotomy, its evolution, its capabilities and limitations, and future directions for its application. I first became interested in the PAO surgery in 1998 while a resident at UC San Diego. I had worked with Dr. Richard Santore who was one of the busiest surgeons in the country performing PAO. I could not believe the incredible results that could be achieved with this elegant procedure. This cultivated my interest in adult reconstructive surgery.
While in Boston at Massachusetts General Hospital in 2002, I reached out to two of the national experts in PAO, Dr. Michael Millis at Boston Children’s Hospital and Dr. Steven Murphy at New England Baptist Hospital and visited them on a number of occasions, observing their technique.


In 2003, the Berne Hip Group, led by Professor Ganz and Dr. Jeff Mast put together an awe-inspiring medical symposium on PAO and Hip Presevation in Mammoth, California.
At that point, I knew that I needed to learn from the master. I was able to secure a fellowship in Berne with Professor Ganz and his highly esteemed associates, Dr. Michael Leunig, Dr. Martin Beck, and Dr. Klaus Siebenrock. I had the opportunity to observe and assist on many PAOs with Professor Ganz and saw hundreds of PAO patients in the clinic.
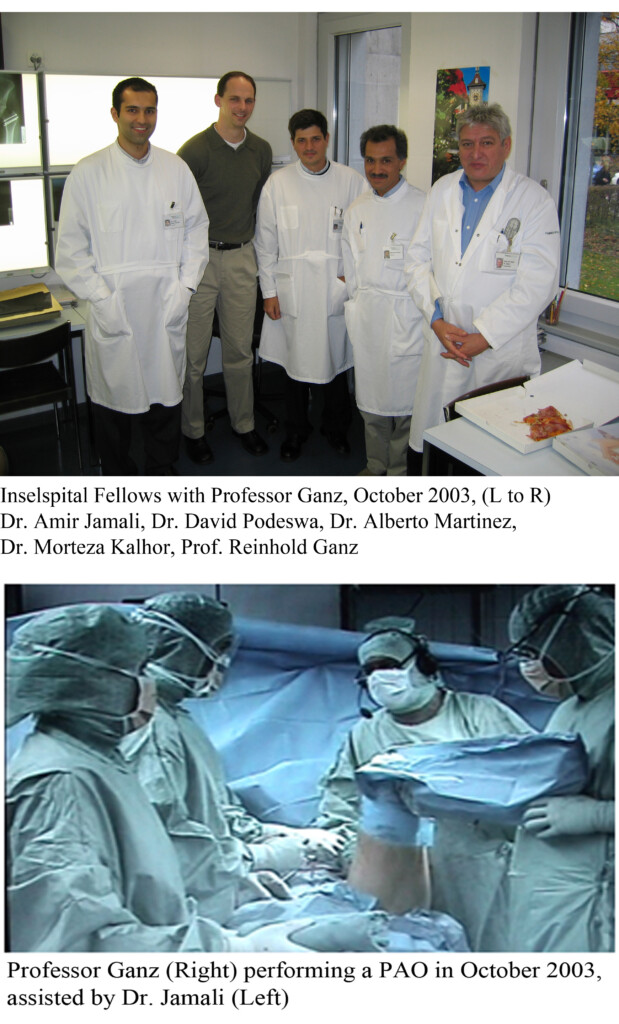
When I returned to the United States, I started doing my own PAOs at UC Davis Medical Center. While at UC Davis, the late Dr. Jeff Mast was a visiting surgeon in 2007 and I had the honor of assisting him in surgery as well.
I have continued to improve the technique and have incorporated more modern planning techniques over the past 15 years. Some of the areas of progress include.
1. Incorporating hip arthroscopy as a precursor operation prior to PAO.
2. Combining PAO with open traction for open hip labrum repair.
3. Performing PAO in combination with surgical dislocation.
4. Preoperative planning of PAO in a 3D environment.
5. Combining PAO with cartilage repair in the hip.
Current research in our lab focuses on the preparation of rapid prototype cutting guides that are custom made to each patient and which allow for minimal x-ray exposure and precise correction of deformity.
Professor Ganz has detailed his experience with PAO in a number of presentations. In summary, very few hip reorientations were done in the 10 years prior to the development of the PAO. Dr. Mast was his research fellow and performed the cadaveric work in developing the PAO in Paris. This culminated int the first PAO surgery performed in 1983. That surgery was performed not for hip dysplasia but rather for another condition called proximal femoral focal deficiency (PFFD). Later the potential for PAO in treating hip dysplasia was discovered.
One of the most important papers on the topic of hip arthritis was put forth by Harris and Stulberg as well as others that hip arthritis was not a primary disease but rather a secondary consequence of structural problems in the hip such as hip dysplasia and hip impingement (termed at the time based on the radiographic appearance of the femur called a “pistol grip deformity”. Murphy and Ganz expanded on this in a landmark paper called “The Prognosis in Untreated Dysplasia of the Hip.” They looked at a large number of patients undergoing hip replacement and evaluated their other hip. They compared the contralateral hips that developed arthritis with those that did not. They found that the ones that developed arthritis commonly had hip dysplasia. This provided strong evidence for the role of dysplasia in developing hip arthritis. An excellent review of this topic is available in this open source article which can be downloaded.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2505145/
With the PAO, a number of studies have shown that not only is hip pain eliminated or greatly reduced, the actual progression of the hip toward arthritis can be altered.
